Menu
Anal fistula is a painful and recurring condition that affects daily life. Many patients feel confused when they hear different surgical terms like fistulotomy and fistulectomy. They often ask — which procedure is better? Which one has less pain? Which one has lower recurrence According to Dr Samrat Jankar, the right procedure depends on the type, location, and complexity of the fistula. There is no “one-size-fits-all” treatment. Proper evaluation is the key to long-term success. This blog explains the difference between fistulotomy and fistulectomy in simple words to help you understand which option may be suitable.
What is an Anal Fistula?
An anal fistula is an abnormal tunnel that forms between the anal canal and the skin near the anus. It usually develops after an abscess (pus infection). If the infection does not heal completely, a fistula forms.
Common symptoms include:
- Pain near the anus
- Persistent discharge
- Swelling
- Recurrent abscess
- Irritation
Surgery is the main treatment. The two commonly performed procedures are fistulotomy and fistulectomy.
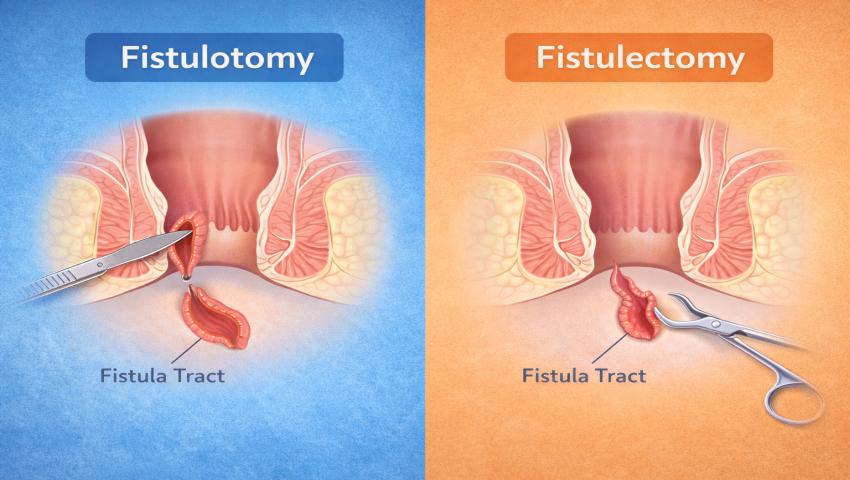
What is Fistulotomy?
Fistulotomy is the most common procedure for simple fistulas. In fistulotomy, the surgeon opens the entire fistula tract. The tunnel is laid open and allowed to heal naturally from inside out.
When is it recommended?
- Simple fistulas
- Low fistulas (not involving much muscle)
- Single tract fistulas
Advantages:
- High success rate
- Lower recurrence in simple cases
- Technically simpler procedure
Disadvantages:
- Open wound healing takes time
- Mild discomfort during healing
- Not suitable for complex or high fistulas
Dr Samrat Jankar recommends fistulotomy when the fistula is straightforward and does not involve a large portion of anal muscles.
What is Fistulectomy?
Fistulectomy involves complete removal of the fistula tract. Instead of opening the tract, the entire tunnel is surgically cut out and removed.
When is it recommended?
- Recurrent fistulas
- Complex tracts
- When complete removal is necessary
Advantages:
- Removes infected tissue completely
- Useful in certain complex cases
Disadvantages:
- Larger wound compared to fistulotomy
- Longer healing time
- Slightly higher risk of muscle damage if not done carefully
Because fistulectomy removes tissue completely, wound size is usually bigger than fistulotomy.
Key Differences Between Fistulotomy and Fistulectomy:
The decision depends on careful clinical examination and imaging like MRI pelvis.
Which Procedure Is Right for You?
There is no universal answer. The correct procedure depends on:
- Location of fistula
- Number of tracts
- Involvement of anal sphincter muscles
- Previous surgery history
- Presence of infection
- Underlying conditions like diabetes or Crohn’s disease
An experienced colorectal surgeon carefully evaluates these factors before recommending treatment.
According to Dr Samrat Jankar, preserving anal sphincter muscle is very important to prevent complications like incontinence. Therefore, selecting the right procedure is crucial.
Are There Other Modern Options?
Yes. Apart from fistulotomy and fistulectomy, advanced options include:
- Laser fistula treatment (FiLaC)
- LIFT procedure
- VAAFT (Video Assisted Anal Fistula Treatment)
- Seton placement for complex fistulas
These sphincter-saving procedures are often preferred for complex or high fistulas.
Dr Samrat Jankar focuses on modern, minimally invasive techniques to reduce pain, speed up recovery, and lower recurrence rates.
Recovery After Surgery:
Recovery depends on the type of surgery performed.
Common post-operative advice includes:
- Regular sitz bath
- High-fibre diet
- Proper hygiene
- Pain control medicines
- Regular follow-up visits
Most patients can resume routine activities within a few days, depending on the procedure.
Proper wound care is very important to prevent recurrence.
When Should You Consult a Specialist?
Seek medical advice if you notice:
- Persistent discharge near anus
- Recurrent abscess
- Pain or swelling
- Previous failed fistula surgery
Early treatment prevents complications and improves success rates.
Final Conclusion:
Both fistulotomy and fistulectomy are effective treatments for anal fistula. The right choice depends on the type and complexity of the fistula. Simple fistulas are often treated successfully with fistulotomy. More complex or recurrent cases may require fistulectomy or advanced techniques. The most important factor is choosing an experienced colorectal specialist who can accurately diagnose and recommend the correct procedure. If you are suffering from anal fistula, consult Dr Samrat Jankar for expert evaluation and personalised treatment. Proper planning ensures better healing and long-term relief.
Recent News

Fistulotomy vs. Fistulectomy: Which Procedure is
16th February 2026
Complex Fistula Management: Why Specialized Surgical
5th February 2026
MRI Fistulogram: The Gold Standard for
27th January 2026
Importance of a Second Opinion for
9th January 2026
Why Recurrent Anal Abscess Often Means
30th December 2025
How Chronic Constipation Damages the Anal
26th December 2025
How Hard Stools Damage the Anal
23rd December 2025
Why Does an Anal Abscess Recur?
22nd December 2025
Top 8 Foods to Avoid When
29th November 2025
MRI for Fistula-in-Ano: Why It’s the
19th November 2025Location
Contact info
- Kaizen Gastro Care, Shop no. 208 / 209, Oriana Crest building, Datta mandir road, Opposite Costa Rica society, Wakad, Pune - 411057
- gastrosamrat@gmail.com
- 097636 35252 / 075584 23708
Fistula Cure
Quick links
© 2026 Kaizen Fistula Care All rights reserved

